Canine Eye Conditions
A quick eye exam on your pet while petting, grooming or even when relaxing on your lap can clue you into any discharge, cloudiness or inflammation of the eyes that may indicate a health problem.
When to Visit Veterinary Eye Institute
Any of the following signs are cause for a visit to the veterinarian, as they can indicate pain, infection or a disease progression:
- Dilated pupils or pupils of two different sizes
- Cloudiness or sudden change in eye color
- Unusual spots on the iris (the colored portion of the eye) or the cornea (the surface of the eye)
- Squinting, winking, or keeping the eye(s) closed
- Pawing at the eye
- Ocular discharge, excessive watering, crustiness in the corners of the eye, tear stained fur
- Visible third eyelid
Why Choose Veterinary Eye Institute
Our ophthalmology team, many of whom are board certified, are dedicated to ensuring that each patient receives the most comprehensive and advanced care possible. We work with other specialties when conditions affect multiple body systems to provide a care plan best suited for your pet’s individual needs. We also partner with your family veterinarian to ensure your pet receives the best, individualized treatment.
In our state-of-the-art facilities, your pet receives the most advanced therapies and procedures available from a team who is consistently at the forefront of veterinary ophthalmology care, research, and technology. This experience and expertise make us a preferred partner for many family veterinarians.
What to Expect During Your Pet’s Eye Exam
When you schedule your appointment, our team will share information on how to prepare for your visit, which may include things like making sure your pet has not eaten (if fasting is required) or bringing a list of their medications.
During your pet’s consultation, our ophthalmology team will review your pet’s medical records from your family veterinarian and discuss your pet’s lifestyle and health history with you. We will perform a comprehensive eye exam on your pet by checking their tear production, measuring eye pressure, and thoroughly examining their eyelids, cornea, lens, retina, and optic nerve.
Based on our findings, your pet may need additional advanced testing. We will discuss your pet’s diagnosis and treatment plan with you and answer any questions you may have. Our team partners with your family veterinarian to provide the best treatment options for your pet.
Commonly Treated Conditions in Dogs

A cataract is an imperfection in the lens of the eye. The lens is inside the eye behind the iris and is responsible for fine focusing of light onto the retina. It should be crystal clear. Any imperfection is referred to as a cataract. Very minor cataracts may have little to no impact on vision but as more of the lens becomes cloudy, vision is compromised. Your pet may experience mild blurring, like looking through dirty glasses. However, if the entire lens becomes opaque, your pet will experience complete blindness.
There are many causes of cataracts in animals. Old age, or senile, cataracts are more commonly seen in people and can occur in animals but do not typically cause problems until very late in life. In dogs we often see cataracts develop at an earlier age (in comparison to people) because of genetic abnormalities. These types of cataracts can develop in dogs as early as one year of age and are typically seen in certain breeds, notably Poodles, Bichon Frises, Havanese, Retrievers, Terriers, Siberian Huskies, and Cocker Spaniels. Mixed breed labradoodles are also commonly affected. Cataracts can also form because of other diseases, particularly diabetes mellitus, and can also appear spontaneously with age or because of intraocular inflammation, trauma, or exposure to certain chemicals.
Once a cataract has progressed to a stage where there is vision impairment there is no way to reverse the cataract. Improving vision will require surgery to remove the cloudy lens. Currently, there is no topical medication that can slow or reverse the progression of cataracts.
Surgical treatment for cataracts may or may not include placing an artificial lens
The most common surgical treatment for cataracts is a procedure called phacoemulsification. Essentially, this means breaking the small lens into small pieces which are then removed from the eye via a small needle. This allows us to perform surgery though a very small (3mm) incision into the eye.
In an otherwise healthy eye, we are also able to implant a new artificial lens. The artificial lens is made of plastic and cannot become cloudy. Placing an artificial lens will restore vision to close to normal, although artificial lenses do not have the ability to change focus like the natural lens does. In some patients we may not be able to place an artificial lens. An eye without a lens can still see well but light is not focused correctly so patients are far-sighted.
Ongoing medical management is important for comfort and quality of life
Left untreated, cataracts continue to leak proteins into the eye. These proteins cause inflammation within the eye and predispose your pet to lens luxation (discoloration of the lens inside the eye), retinal detachment, and/or glaucoma (damage to the optic nerve which leads to blindness). Although retinal detachment is not painful, lens luxation, inflammation, and glaucoma are, and your dog may need pain medication.
If your pet does not have cataract surgery, daily eye drops may be needed for your pet’s comfort. In addition, we recommend your pet receives a complete ocular examination regularly to monitor the cataract progression and maintain their optimal quality of life.

Dry eye is a term we use to describe a group of diseases that results in abnormal tear production. The medical term for dry eye is Keratoconjunctivitis sicca or KCS, which means inflammation of the cornea and conjunctival membranes due to dryness. Dryness of the corneal surface makes vision uncomfortable for your pet and can lead to corneal scarring and ulceration.
Chronic allergies are a common cause of dry eye in dogs
The most common form of KCS is a decrease in watery tears due to inflammation in the tear glands. This is often associated with chronic allergies. The result is a slow decline in tear production causing redness, irritation, and thick green discharge. Tears are very important to the health of the cornea and over time, blood vessels and scarring will develop, and there is risk of a corneal ulcer forming. With severe dry eye the cornea can become severely damaged which can result in permanent vision loss.
There are also lesser common causes of dry eye, including: neurogenic dry eye which typically will affect one eye suddenly, dry eye caused by sulfa drug toxicity, and qualitative dry eye which is a result of abnormal lipid and mucin in the tears.
For most patients, dry eye requires life-long medical management, which includes medications that stimulate normal tear production. For dogs that do not respond to medication therapy there are surgical options for KCS including a parotid duct transposition, buccal mucosal grafting, and episcleral cyclosporine implantation. Your veterinary ophthalmologist will discuss these options with you if your dog is a surgical candidate.

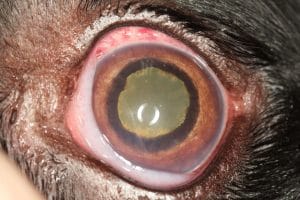
Glaucoma is a disease caused by elevated pressure inside the eye (intraocular pressure or IOP) because of a buildup of fluid in the eye that doesn’t drain properly. The increased pressure can become painful and cause damage to the retina and optic nerve. We categorize glaucoma as either primary (a genetically inherited disease) or secondary (high pressure caused by some other disease).
Primary glaucoma is mostly seen in certain breeds of dogs, including Samoyed, Husky, Basset Hound, Cocker Spaniel, Beagle, Chow Chow, Maltese, Shar Pei, and Shiba Inu.
The disease is a result of the fluid drain inside the eye not developing properly. Most patients will have normal pressure until middle age (5 to 7 years) and then will experience an elevation in pressure, often very suddenly. Early signs are cloudiness in the eye, redness in the white of the eye, squinting, and vision loss. If inherited glaucoma occurs in one eye, the chances of it also developing in the other eye are 50% within 12-18 months; so close monitoring can help detect changes in eye pressure earlier to help maintain vision as long as possible.
Secondary glaucoma stems from any number of other causes such as another disease or an injury to the eye. Uveitis is an inflammatory condition in the eye that can end up blocking the drainage system. Instability of the lens and lens disorders like cataracts where the lens moves out of place and can end up blocking the drainage area or trapping fluid. Retinal detachment, tumors, cancer, or injuries to the eye can also end up causing a blockage.
The goal of glaucoma treatment is to reduce eye pressure and alleviate pain
Unfortunately, there is no cure for glaucoma, but it can be managed for a period if it’s treated properly. The goal of the treatments is to reduce the eye pressure so your dog can be more comfortable. This typically begins with medication in the form of eye drops.
Some medications work to decrease the production of the fluid and others focus on helping the fluid drain better. The effectiveness of the medications and how long they can work to control glaucoma and maintain your pet’s vision varies between patients. Since there is no cure, once medication begins, it will need to continue for the length of your pet’s life.
If medication alone becomes ineffective or if a pet is at a high risk of vision loss, laser surgery may also be used. One surgical option is called Endocyclophotocoagulation or ECPC. During the surgery, a strong beam of light is used to destroy the ciliary processes, the part of the eye that produces the aqueous humor, which then reduces the fluid production in the eye. Another is an Enucleation, which involves removing the eye and sewing the eyelids shut. There are also options that remove parts of the eye and replace them with a prosthesis which offers a cosmetic approach. Yet another is a ciliary body ablation or chemical ablation where the veterinarian injects drugs that try to stop all intraocular fluid production. If done to an eye with vision, this procedure will cause blindness, so a ciliary body ablation is reserved for those that are blind and experiencing pain from the elevated pressure. All surgeries present different risks and those should be discussed with your veterinary ophthalmologist.

Entropion describes a condition in which the eyelids are not positioned correctly, turning inward and allowing hair from the skin to contact and irritate the surface of the cornea. The hair rubbing against the cornea is painful and can cause corneal ulceration and scarring. Ulcers can become vision threatening if secondary infections develop. Chronic entropion can lead to vision loss due to scarring of the cornea.
Entropion can be a result of several factors including an eyelid that is too long, prominent nasal folds in certain breeds, excess forehead skin or significant muscle loss in older patients.
Treatment of entropion usually requires surgery to correct the underlying abnormalities. This often involves shortening and rolling the eyelid outward. Correction of excess nasal folds or forehead skin may also be required in more severe cases.

Cherry eye is the layman’s term for a prolapsed third eyelid gland. The third eyelid gland is one of the two glands that provide tears to each eye. Then third eyelid gland is normally anchored to cartilage at the base of the third eyelid (an extra membrane present in most animals). In some animals, particularly certain breeds, there is an abnormality in the attachments of the gland to the cartilage. This allows the gland to come free and prolapse out of the normal position. The gland is usually visible as a red mass at the inner corner of the eye.
When the gland is out of position it will often become inflamed and irritated, it will prevent normal blinking which can result in damage to the cornea. Over time the gland will become scarred and non-function resulting in a decrease in tear production. This can lead to corneal damage and vision loss.
The best treatment for this condition is surgery to replace the gland into a more normal position. There are several techniques to accomplish this, and the recommended technique will vary by patient. In the hands of a trained ophthalmologist the success rate of surgery is typically in the 95-98% range.
Uveitis describes inflammation of vascular tissue inside the eye consisting of the iris, ciliary body, and choroid. Symptoms of uveitis can include cloudiness, squinting, redness in the white of the eye and changes in vision. Inflammation of these tissues can result in severe damage to the eye including glaucoma, cataract formation, retinal detachment, and bleeding inside the eye. All of these can lead to permanent vision loss.
There are many causes of uveitis including infectious diseases, cancers, and autoimmune disease. Causes of uveitis in dogs include:
- Tick born diseases such as Erhlichia, Rocky Mountain Spotted Fever, Rickettsia, and Lyme Disease.
- Fungal infections such as Blastomycoses, Histoplasmosis, Cryptococcosis, or Coccidiomycosis.
- Parasitic disease due to intestinal parasites or heartworm disease.
- Neoplasia (cancer) of the eye, or cancer of another area of the body that has spread to the eye.
- Immune-mediated (like Lupus or Rheumatoid arthritis in people), the body’s own immune system begins to attack the uvea, causing inflammation throughout the eye. This is a diagnosis of exclusion (rule out other causes) and usually responds well to treatment, but lifelong therapy is required to maintain control.
Regardless of the cause, uveitis requires treatment to try to prevent secondary glaucoma, permanent blindness, and pain. Additionally, given the nature of this condition, diagnosing a specific cause of uveitis will often require special testing and the prognosis will depend on the underlying cause.

A corneal ulcer occurs when the cells which cover the surface of the cornea are damaged leaving an open wound. Ulcers are typically very painful, and symptoms usually include squinting, tearing and rubbing at the eye.
We often describe ulcers as being simple or complicated. Simple ulcers may occur from minor trauma to the eye. Once injured the corneal cells will rapidly regenerate and heal within a few days. The major concern with a corneal ulcer is development of a secondary infection. Treatment for simple ulcers is supportive care, use of antibiotics to prevent infection, pain control, and a protective e-collar to prevent rubbing.
Ulcers are considered complicated if they are not healing in an appropriate amount of time or when there is an identifiable external cause to the ulcer. External causes include hair rubbing on the cornea from abnormal eyelid conformation, abnormal hairs present underneath the eyelid, foreign bodies and low tear production. Secondary infections will also complicate ulcers and can result in loss of corneal tissue which risks loss of the eye or compromised vision.
Another common complicated ulcer is called a refractory, or non-healing ulcer. This is a common disease of older dogs, particularly of certain breeds in including Boxer’s and Pit Bull type breeds. This condition results from abnormal attachments of the surface cells to the corneal collagen. These ulcers will typically not heal without performing a procedure to the cornea to stimulate proper cell attachment.
The most important thing when treating corneal ulcers is identifying any underlying cause and addressing it to prevent vision loss.
- rapid development of cataracts
- glaucoma
- retinal detachments
- inflammation of the retina or optic nerve
- severe inflammation in the front of the eye
- central nervous system disease.
The expert, compassionate team at VEI can typically identify the cause of vision loss with an eye exam. However, some diseases may require additional testing.
If your pet is experiencing significant changes in vision, we recommend scheduling an appointment as soon as possible. You can call the nearest VEI location directly or ask your family veterinarian for a referral.
We encourage you to contact your family veterinarian or the nearest emergency veterinary hospital if you feel your pet is experiencing a medical emergency.